Explore the connection between the gut microbiome and mental health. Learn how the gut-brain axis, probiotics, and diet influence mood, anxiety, and depression.
The Link Between Gut Microbiome and Mental Health
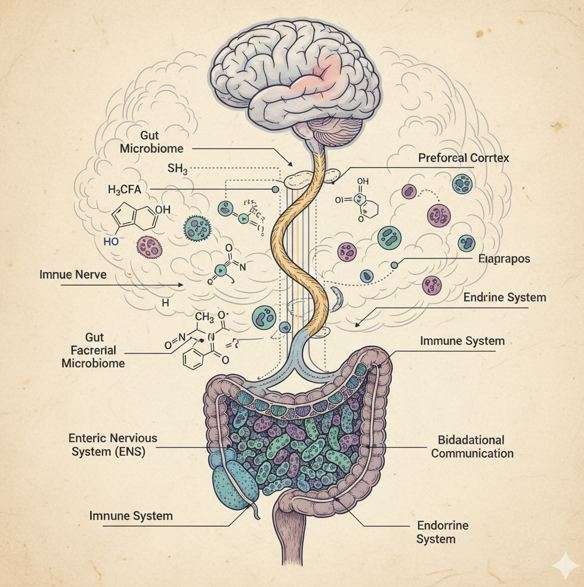
The gut is often called our “second brain”, and modern science shows this nickname is more accurate than ever. Trillions of microorganisms living inside the digestive system—collectively known as the gut microbiome—do far more than help with digestion. They play a crucial role in immunity, metabolism, and even mental health. In recent years, researchers have uncovered fascinating links between gut bacteria, mood regulation, and psychiatric conditions such as anxiety and depression.
This article explores how the gut microbiome and mental health are connected through the gut-brain axis, what the latest research says, and how diet and probiotics may support emotional well-being.
👉 Harvard Health Publishing – The gut-brain connection
The Gut-Brain Axis: A Two-Way Communication
The connection between the gut and the brain is called the gut-brain axis. It is a complex communication network that uses nerves, hormones, and immune pathways to send signals both ways. When the gut microbiome is balanced, it sends positive signals to the brain, supporting calmness and emotional stability. However, when the gut is imbalanced—a condition called dysbiosis—it can increase inflammation, disrupt brain signaling, and contribute to stress, anxiety, and mood swings.
Importantly, some gut microbes produce neurotransmitters such as serotonin, dopamine, and GABA. These chemicals regulate mood and emotions, and disruptions in their production may worsen mental health issues.
What Research Reveals About Gut Microbiome and Mental Health
Recent studies show that individuals with depression and anxiety often have less diverse gut bacteria. For example:
- A reduction in beneficial short-chain fatty acid (SCFA)–producing bacteria, such as those generating butyrate, has been linked to higher risk of mood disorders.
- Some harmful bacteria increase inflammation, which can affect brain function.
- Probiotics—beneficial live bacteria found in yogurt, kefir, and supplements—may reduce stress hormones and improve mood.
- A systematic review published in Nature highlighted that changes in the gut microbiome are consistently observed in patients with depression and schizophrenia, suggesting that the microbiome may be a key factor in psychiatric health.
- 👉 For further reading, check out Harvard Health Publishing – The gut-brain connection
Mechanisms Linking Gut and Brain
The influence of the gut microbiome on mental health occurs through several pathways:
- Neurotransmitter Production: Certain gut bacteria manufacture serotonin and dopamine, the same chemicals targeted by antidepressant drugs.
- Immune Regulation: Dysbiosis can cause a “leaky gut,” allowing toxins and inflammatory compounds into the bloodstream. These can reach the brain, triggering neuroinflammation linked to depression.
- Stress Response: The microbiome affects the hypothalamic-pituitary-adrenal (HPA) axis, which regulates cortisol, the primary stress hormone. An imbalanced microbiome may exaggerate stress responses.
Supporting Gut Microbiome and Mental Health
- The good news is that you can support both gut and mental health through simple lifestyle choices:
- Eat a Fiber-Rich Diet – Whole grains, fruits, vegetables, and legumes promote microbial diversity.
- Include Fermented Foods – Yogurt, kefir, kimchi, and sauerkraut contain live probiotics that nourish the gut.
- Try Prebiotics and Probiotics – Prebiotics (fibers that feed good bacteria) and probiotics (live bacteria) together create a healthier gut environment.
- Limit Processed Foods – Diets high in sugar and processed products promote dysbiosis, which may worsen mood swings.
- Stay Physically Active – Exercise has been shown to increase beneficial gut bacteria and improve mental health.
- 👉 For more on probiotics, see NIH – Probiotics: What You Need To Know.
Future Directions: Microbiome-Based Therapies
As research progresses, scientists are exploring advanced treatments such as:
- Personalized Probiotic Therapy – Using microbiome sequencing to tailor supplements to an individual’s unique gut profile.
- Fecal Microbiota Transplantation (FMT) – Though still experimental, FMT is being studied as a possible therapy for psychiatric conditions.
- Precision Nutrition – Designing diets based on one’s microbiome to improve both physical and mental health.
- While these therapies are still under study, early results suggest that balancing the gut could one day become part of mainstream psychiatric treatment.
Final Thoughts
The evidence is clear: the gut microbiome and mental health are deeply connected. From neurotransmitter production to stress regulation, gut microbes influence how we think, feel, and respond to daily challenges. Supporting your gut through a balanced diet, probiotics, and healthy habits is not only good for digestion but also for your emotional well-being.
As science evolves, we may soon see gut-friendly therapies standing alongside counseling and medication in the treatment of anxiety and depression. Until then, remember—to nurture your mind, don’t forget to nurture your gut.